Journal of APPLIED BIOMEDICINE
ISSN 1214-0287 (on-line)
ISSN 1214-021X (printed)
Volume 11 (2013), No 3, p 187-193
DOI 10.2478/v10136-012-0021-z
Tacrine can suppress immunity response to tularemia in BALB/c mouse model
Miroslav Pohanka, Oto Pavlis
Address: Miroslav Pohanka, Faculty of Military Health Sciences Brno, University of Defense, Trebesska 1575, 500 01 Hradec Kralove, Czech Republic
miroslav.pohanka@gmail.com
Received 17th September 2012.
Revised 12th October 2012.
Published online 15th October 2012.
Full text article (pdf)
Summary
Key words
Introduction
Material and Methods
Results
Discussion
Conclusions
Acknowledgements
References
SUMMARY
Tacrine is an inhibitor of enzyme acetylcholinesterase (AChE). In the past, it was used for the treatment of cognitive dysfunction during vascular dementia and Alzheimer disease. Some works have concluded that AChE inhibitors can modulate immune response, and for this reason, we decided to investigate the immune response to a model bacterial disease - tularemia - for which both innate and specific immunity are necessary to resolve the disease. We used 64 BALB/c mice divided into eight groups exposed variously to saline, tacrine in a dose of 20.0-500 microg/kg, infection with tularemia and infection with the contemporary application of tacrine. The mice were euthanized three days after the start of the experiment. We proved a significant reduction in the levels of interleukin-6 (IL-6) and interferon gamma (IFN-gamma) in a dose response manner in the infected animals in the course of tularemia. Moreover, tacrine caused a significant increase of the bacterial burden in the liver and spleen. We can conclude that tacrine can aggravate tularemia: that it increases the accessibility of acetylcholine and in this way stimulates the cholinergic anti-inflammatory pathway. The results represent a substantial contribution to the field of inflammation control in the nervous system and it is an advancement of the inflammatory therapy issue.
KEY WORDS
inflammation; infection; Alzheimer disease; tacrine; acetylcholinesterase; innate immunity
INTRODUCTION
Tacrine (9-amino-1,2,3,4-tetrahydroacridine) is an inhibitor of both AChE (EC 3.1.1.7.) and butyrylcholinesterase (BChE; EC 3.1.1.8.). In the cholinesterases, tacrine binds to the α-anionic site in the active center of the enzymes. Though it inhibits both the cholinesterases, a higher affinity to AChE is reported (Ahmed et al. 2006, Pohanka 2011b). In the past, tacrine was marketed under its trade name Cognex and was used for the treatment of cognitive dysfunctions in Alzheimer disease and related vascular dementias. Despite its high efficacy, tacrine was withdrawn from clinical use because of metabolic activation causing adverse effects in the liver (Alfirevic et al. 2007, Pohanka 2011a, 2012a).
When used for Alzheimer disease therapy, tacrine was given to improve acetylcholine insufficiency (Krall et al. 1999). In later research, the association of inflammation via IL-6 in tacrine induced hepatotoxicity has been reported (Carr et al. 2007). On the other hand, tacrine was found to abolish lipopolysaccharide induced inflammation including IL-6 secretion in the central nervous system (Tyagi et al. 2007). The findings are supported by our recent experiments with another inhibitor of AChE - neostigmine (Pohanka and Pavlis 2012). In the present experiment, we decided to investigate the potential implication of tacrine in immunomodulation of an infectious disease. The results illustrate the effect of tacrine in chronic inflammatory disorders including Alzheimer disease. We chose tularemia, a disease caused by Francisella tularensis, as a model disease since both innate and adaptive immunity are necessary for the resolution of the disease and macrophages play a crucial role in the immunity reactions (Fernandes-Alnemri et al. 2010, Mahawar et al. 2012). Because of the work of other authors quoted here we assume a modulation of the immune response to tularemia by tacrine and the present experiment is devoted to the elucidation of this effect. The understanding of this is helpful not only for identification of the biological effects in the organism but also for the use of the extrapolated results in understanding the role of AChE inhibitors in pathogeneses associated with inflammatory processes.
MATERIAL AND METHODS
Microorganism
F. tularensis LVS (strain ATCC 29684) was chosen for the experiment. The microorganism was cultivated in a standard manner on McLeod agar supplemented with hemoglobin from bovine blood (Sigma-Aldrich, Sigma-Aldrich, St. Louis, MO, USA) and Iso VitaleX (Becton-Dickinson, San Jose, CA, USA) at 37 °C. After one day, the culture was harvested using a disposable plastic scraper. The scraped cells were re-suspended in saline solution and then washed by centrifugation at 2,000 x g for 10 minutes. The exact concentration of viable cells was confirmed by a cultivation test as described above.
Laboratory animals
A total of 64 BALB/c laboratory mice (Velaz, Unetice, Czech Republic) were received in their sixth week and they were used for the purposes of the experiment after another two weeks of quarantine. We chose BALB/c as an optimal animal model as the mice are frequently used for tularemia pathogenesis research by other scientists (Shen et al. 2010). Thus the experimental data are also easily comparable to our previous results (Pohanka and Pavlis 2012). At the beginning of the experiment, the animals weighted 21±1 g. For the whole period of the experiment, the animals were kept in an air conditioned laboratory with temperature 22±2 °C, humidity 50±10%, and continuous 12 hour periods of alternating dark and light. Food and water were supplied to the animals without limitation. The experiment was properly approved by the ethical committee of the Ministry of Defence (Czech Republic) and all manipulations of the animals including euthanasia were carried out in an accredited vivarium of the Centre of Biological Defense in Techonin (Czech Republic).
Laboratory animals experiment performance
The animals were divided into 8 groups of 8. Saline, bacterial suspension in saline and tacrine hydrochloride hydrate (99% purity; Sigma-Aldrich) were given in amounts of 100 microl subcutaneously into the rear limbs. The F. tularensis concentration used in the experiment was 2.91 x 106 CFU/ml. freshly confirmed in a cultivation test, The Tacrine was solved in order to be given in doses 0.02-0.1-0.5 mg/kg from which the doses 0.1-0.5 mg/kg were derived from the previously noted therapeutic doses for Alzheimer’s disease patients (Davis et al. 1992, Knapp et al. 1994). In the experiment described, the animals receiving tacrine were challenged by the same dose of the drug the second day after the beginning of the experiment. Eight groups were subsequently established: 1. controls receiving saline only; 2. tacrine 0.02 mg/kg first and second day; 3. tacrine 0.1 mg/kg first and second day; 4. tacrine 0.5 mg/ kg first and second day; 5. infection by F. tularensis; 6. infection by F. tularensis and tacrine 0.02 mg/kg first and second day; 7. infection by F. tularensis and tacrine 0.1 mg/kg first and second day, and 8. infection by F. tularensis tacrine 0.5 mg/kg first and second day. The animals were euthanized after three days using CO2 anaesthesia and heart puncture. Blood was collected into tubes with adsorbed lithium heparin (Dialab, Prague, Czech Republic). Spleens and livers were sampled from cadavers immediately after blood collection.
Ex vivo assay
The freshly collected blood was centrifuged at 1,000 x g for 5 minutes and plasma was separated. The plasma samples were processed using an indirect enzyme linked immuno-sorbent assay (ELISA) for the determination of IL-6 and IFN-gamma. Kits from Abcam Company (Cambridge, MA, USA) developed for standard 96 wells microplates were used. The kits were processed in compliance with printed and attached instructions.
The spleens and livers were homogenized immediately after collection by passing through nylon net with holes sized 1 mm2. The homogenate was re-suspended into saline and spread over the McLeod agar with composition as reported above. The agar was incubated in a way previously described and colonies were counted two days after incubation beginning.
Statistical analysis
The achieved data were processed in Origin 8 Pro (OriginLab Corporation, Northampton, MA, USA) software using the one-way ANOVA test and the Bonferroni test at the significance level 2alpha=0.05.
RESULTS
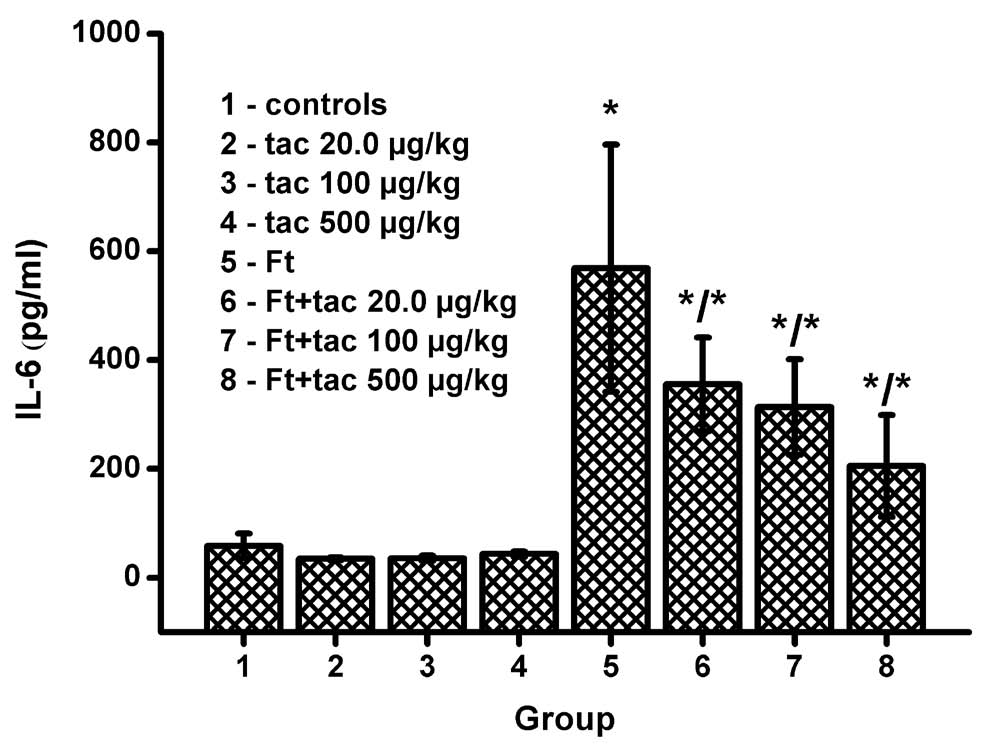
The IL-6 level is depicted in Fig. 1. Tacrine alone did not cause any alteration in the cytokine level when compared to the controls. The infected animals had significantly increased IL-6. Tacrine was able to significantly reduce the IL-6 level and the reduction was in a dose response manner. Three days into the experiment, the IL-6 level had increased from 58 pg/ ml (controls) up to 569 pg/ml in the tularemia infected animals (group 5). The upper dose of tacrine in the infected animals (group 8) significantly reduced IL-6 level up to 205 pg/ml.
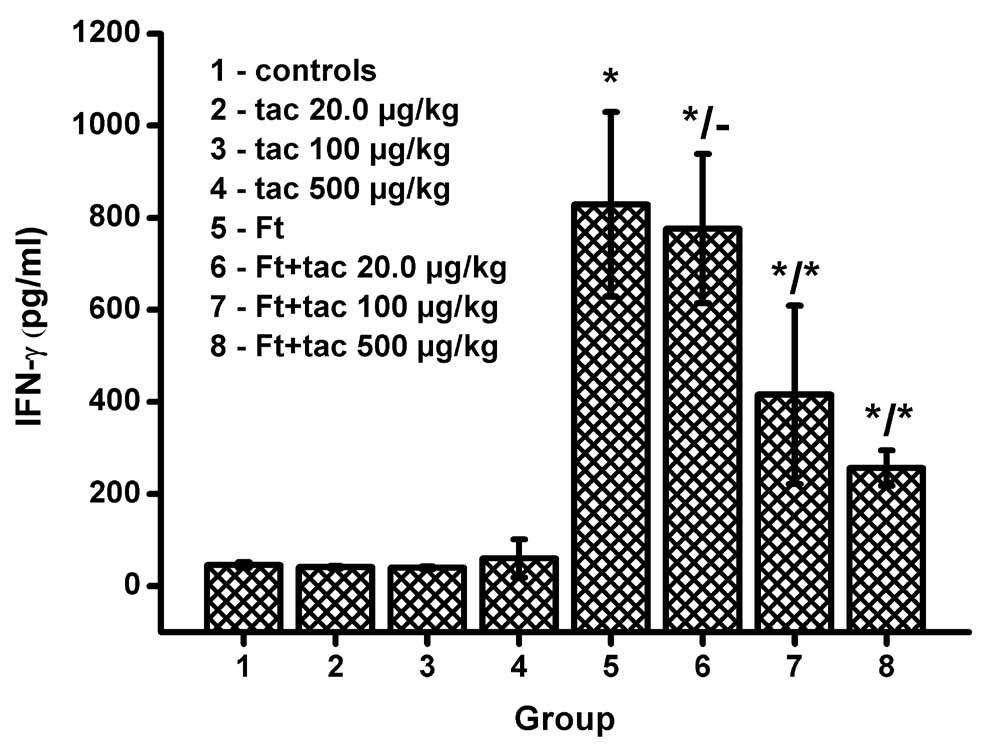
The second assayed cytokine was IFN-gamma. Levels of the marker are depicted in Fig. 2. The cytokine levels did not alter in the groups administered with tacrine where the animals were not infected (groups 2-3). Theeapplication of tacrine into the tularemia infected mice caused the decrease of IFN-gamma in a dose response manner. The lowest dose of tacrine, 20.0 microg/kg, did not cause a significant decrease of IFN-gamma. However, the doses of tacrine 100 and 500 microg/kg initiated a significant decrease of IFN-gamma; level in the course of tularemia.
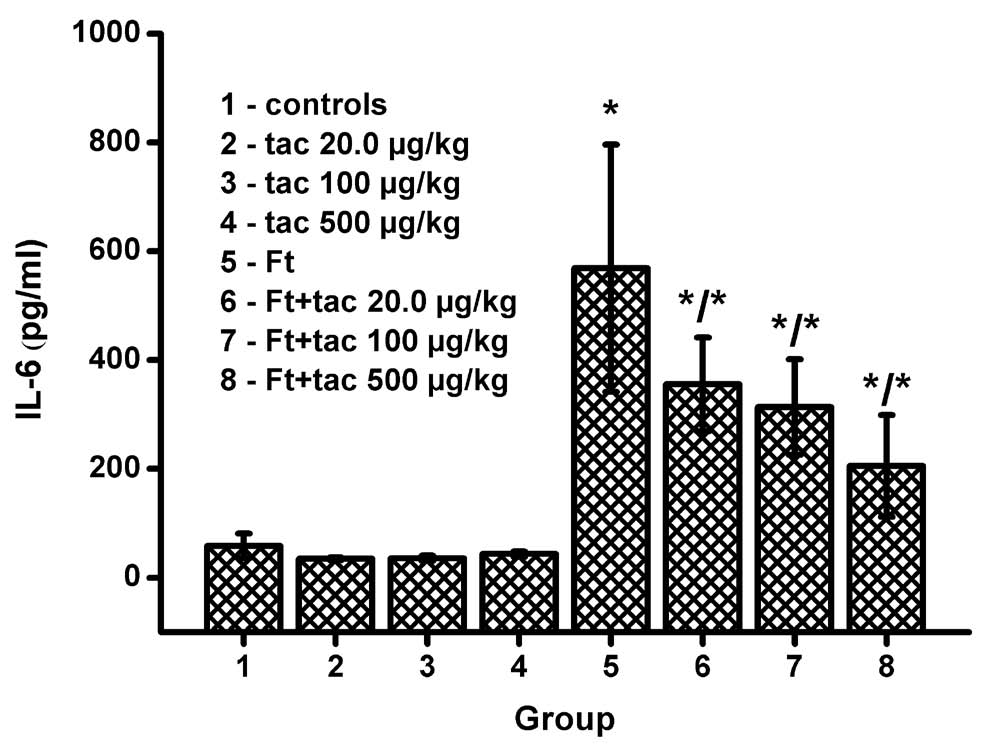
Fig. 1. Level of interleukin-6 (IL-6) in plasma samples. Composition of groups is depicted in the figure. Error bars indicate standard deviation for a group sized eight specimens. Asterisk in group 5 respective asterisk in numerator for groups 6-8 respond to significance against group 1. Asterisks in denominator of groups 6-7 responds to significance against group 5.
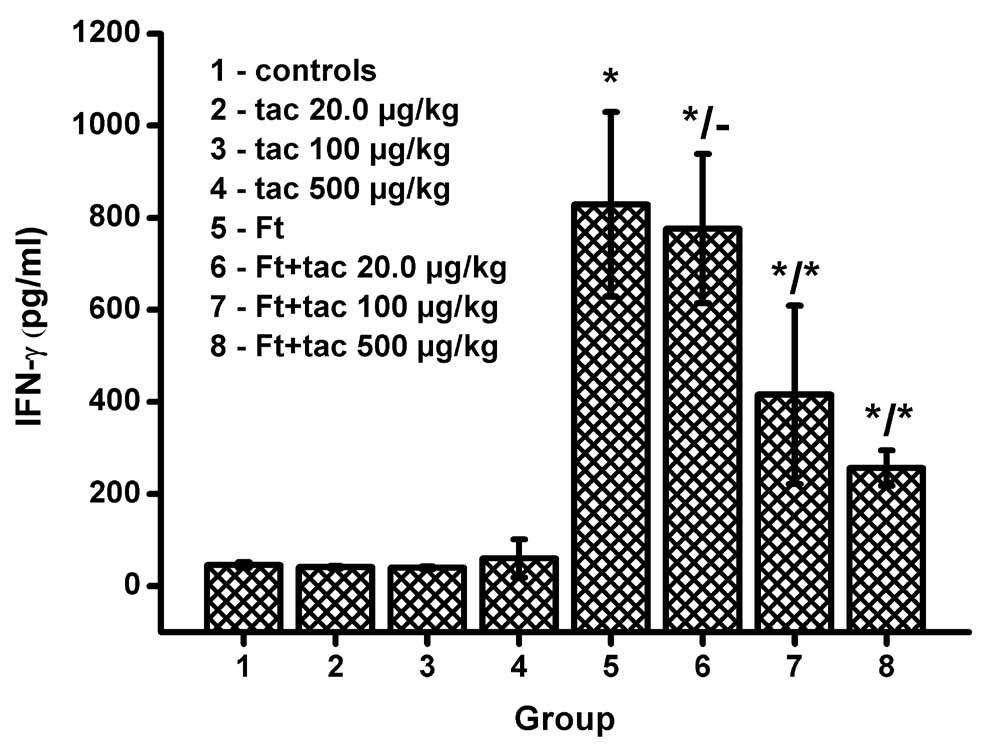
Fig. 2. Level of interferon gamma (IFN-gamma) in plasma samples. Description is same as provided in the Fig. 1.
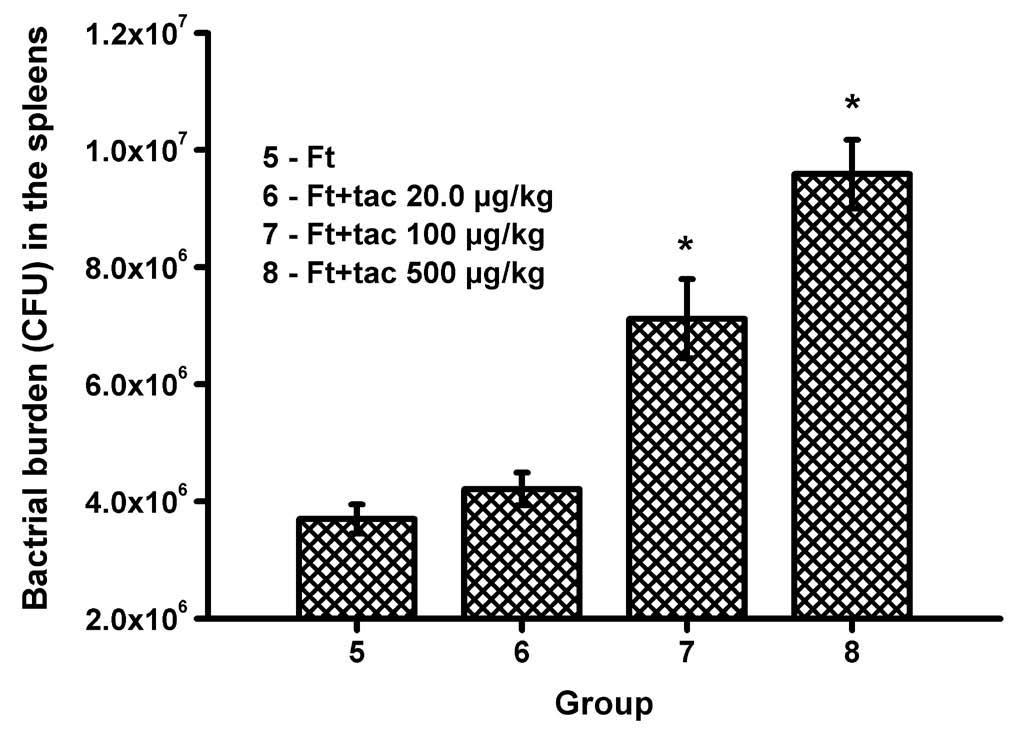
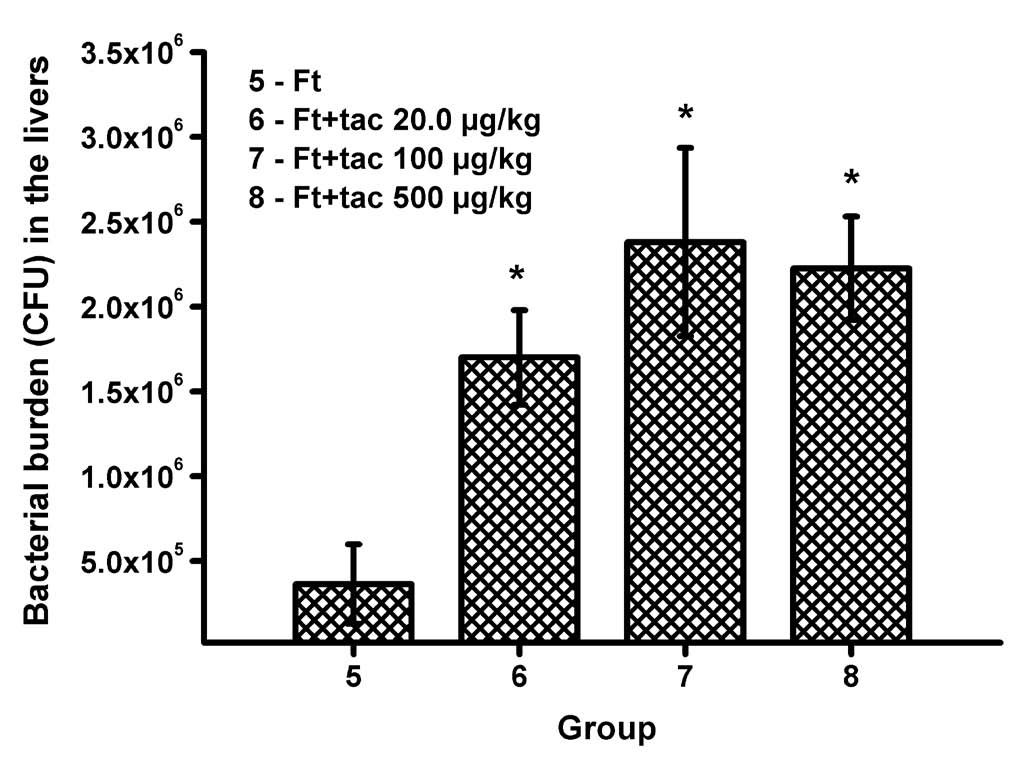
The bacterial burden in the organs examined was influenced by application of tacrine. The total number of bacteria increased in a dose response manner in both liver and spleen. The increase was more extensive in the liver than in the spleen. When compared to the non treated and infected animals only, the highest dose of tacrine caused approximately 2.5 times the increase of bacterial burden in the spleen and 5 times increase in the liver. In compliance with expectation, the non infected animals (groups 1-4) had no microbiological findings in either the liver or spleen.
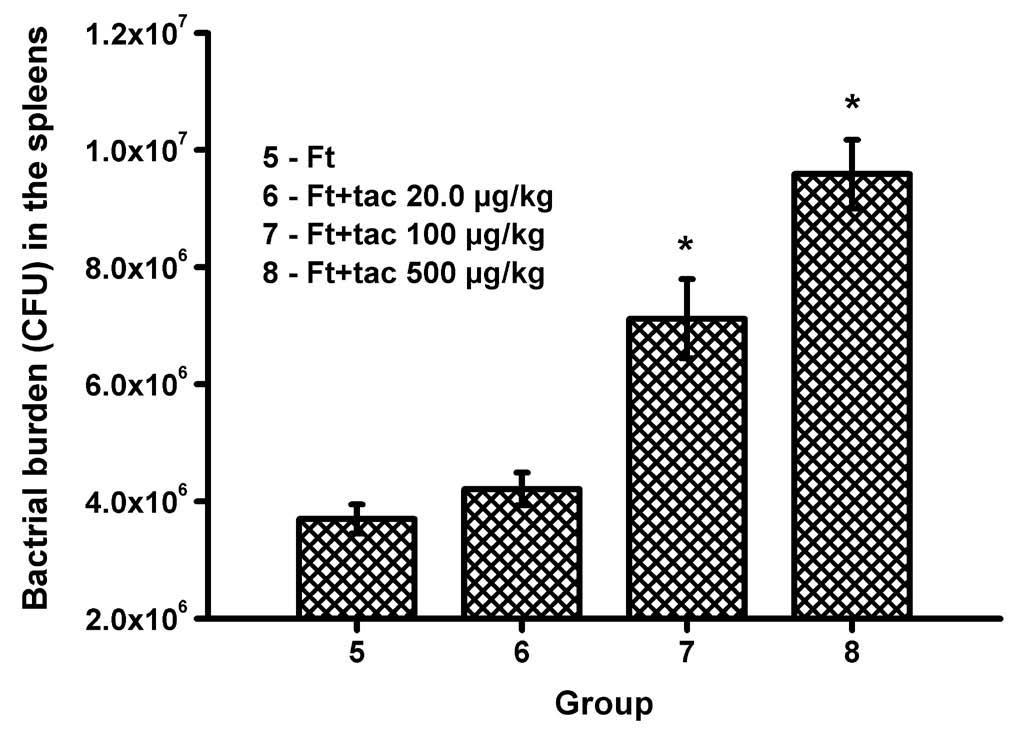
Fig. 3. Bacterial burden in spleens of the infected animals. Composition of groups is depicted in the figure. Error bars indicate standard deviation for a group sized eight specimens. Asterisk indicates significance against group 5.
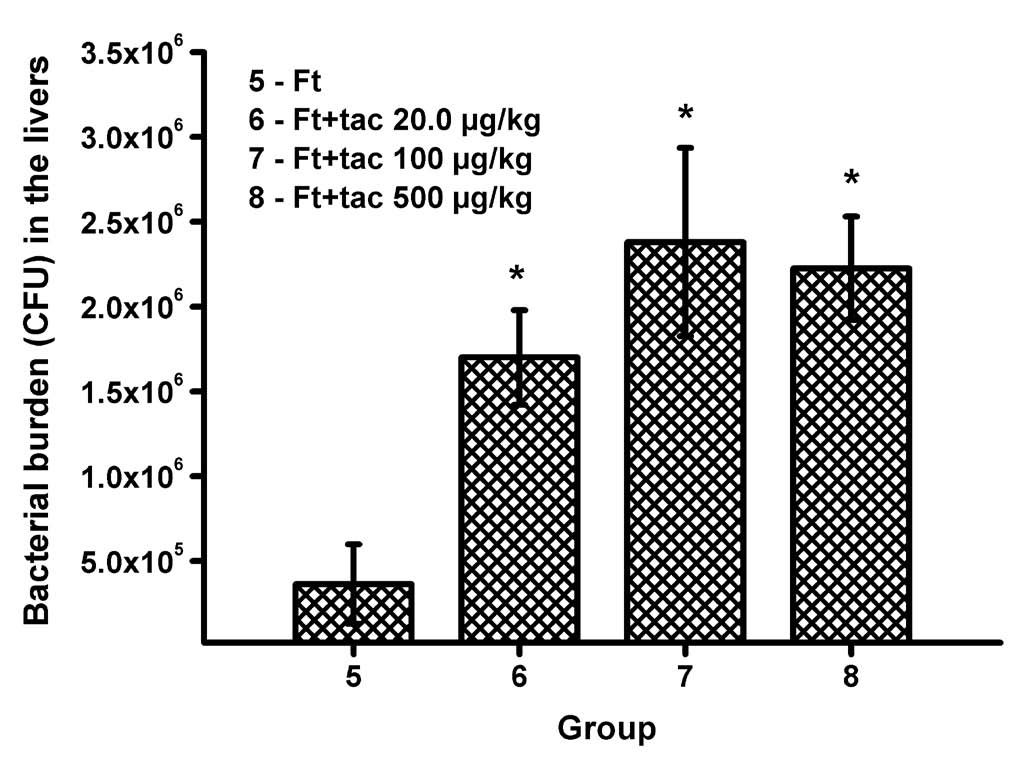
Fig. 4. Bacterial burden in livers of the infected animals. Description is same as provided in the Fig. 3.
DISCUSSION
The time interval of euthanasia was chosen in compliance with our previous results and findings from quoted papers (Chiavolini et al. 2008, Pohanka
et al. 2012). The three day period from the start of infection to euthanasia was chosen as optimal because innate immunity is sufficiently activated and the level of inflammatory cytokines and bacterial burden culminate (Pohanka et al. 2012). On the The time interval of euthanasia was chosen in other hand, pertinent deaths could happen later and compliance with our previous results and findings the expected level of IFN-gamma had already increased from quoted papers (Chiavolini et al. 2008, Pohanka enough to be measurable (Chiavolini et al. 2008, et al. 2012). The three day period from the start Pohanka et al. 2012). The cytokines were chosen of infection to euthanasia was chosen as optimal to provide knowledge about both innate immunity because innate immunity is sufficiently activated and and anti-intracellular pathogen immune responses. IL-6 is a cytokine released from macrophages in a large scale during inflammation and it is useful for research on the cholinergic anti-inflammatory pathway (Wilund et al. 2009). We used an assay of IL-6 for the reason mentioned. IFN-gamma was the second assayed marker. The cytokine is a crucial part in both the innate and adaptive immunity. Moreover, it activates macrophages during an infection so positive feed-back is constituted. Release of IFN-gamma during tularemia is a crucial factor for resolving the disease by macrophages (Novosad et al. 2011).
Because of these results, we can assume that tacrine can aggravate tularemia progression. The process is, however, more complicated than this. Tacrine is an inhibitor of both AChE and BChE and it is able to simply cross the blood brain barrier and act not only in the peripheral nervous system but in the central nervous system as well (Teltingdiaz and Lunte 1993). It is unlike carbamate inhibitors which act dominantly in the peripheral nervous system and do not go into the brain (Jokanovic 2009) or penetrate under specific conditions such as stress (Friedman et al. 1996). On the other hand, the results for tacrine point to a process close to the previously described findings for carbamate neostigmine (Pohanka and Pavlis 2012) and a paper written by Wang and coworkers also contains findings about the suppression of immunity including inflammation after the application of a cholinesterase inhibitor: huperzine (Wang et al. 2012). The correlation of results indicates the same mechanism of action for the compounds mentioned. We can infer that the tacrine immunomodulatory effect is based on inhibition of cholinesterases in the peripheral nervous system.
The most probable explanation of the phenomenon found is that the compounds meet the cholinergic anti-inflammatory pathway. The pathway consists of the nervus vagus termination in the blood system and alpha7-nicotinic acetylcholine receptor (alpha7 nAChR) on macrophage surfaces (Zitnik 2011). The stimulation of alpha7 nAChR is quickly terminated by an action of AChE located on erythrocytes (Pohanka 2012b). Inhibition of AChE can improve the accessibility of acetylcholine and in this way induce stimulation of the cholinergic anti-inflammatory pathway. Activation of the nicotinic anti-inflammatory pathway suppresses inflammation during antigenic stimulation of the immune system and the activation can be initiated by direct agonizing of alpha7 nAChR (Chatterjee et al. 2012) or the inhibition of AChE (Sun et al. 2012).
In this experiment, tacrine caused aggravation of the tularemia disease. For this reason, application of tacrine or similarly acting compounds can be considered as a risk factor during bacterial infections. On the other hand, the beneficial action of AChE inhibitors in some pathogeneses can be attributed only to the link with inflammation regulation. The idea is supported by some experimental findings such as the prevention of cognitive deficits due to inflammation when AChE inhibitor galantamine is applied (Field et al. 2012). In another work, epileptogenesis induced by inflammation was suppressed by the application of acetylcholine (Gnatek et al. 2012). Because of previous work in the papers quoted and the results of this experiment reported here, we are led to think that AChE inhibitors can be used for the suppression of inflammation including neuroinflammation. The findings are in good compliance with our previous experiment with neostigmine (Pohanka and Pavlis 2012). Compared to neostigmine, tacrine acts not only in the peripheral nervous system but also in the central nervous system so it might be suitable for the regulation of neuroinflammation.
CONCLUSIONS
Tacrine can aggravate the progress of tularemia in a mouse model. The most probable explanation is that the AChE inhibitor stimulates the cholinergic anti-inflammatory pathway and the suppressed immune system is not easily able to resolve the disease. On the other hand, the effect would be beneficial in several pathologies such as neurodegenerative disorders; e.g. the positive effect of tacrine when used in therapy for Alzheimer's disease would be attributed to its anti-inflammatory action in addition to any improvement in cognitive functions.
ACKNOWLEDGEMENTS
The Ministry of Education, Youth and Sports of the Czech Republic for project LH11023 and Faculty of Military Health Sciences, University of Defence, Czech Republic for A long-term organization development plan 1011 are gratefully acknowledged. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
REFERENCES
Ahmed M, Rocha JBT, Correa M, Mazzanti CM, Zanin RF, Morsch ALB, Morsch VM, Schetinger MRC. Inhibition of two different cholinesterases by tacrine. Chem-Biol Interact. 162: 165-171, 2006.
[CrossRef]
[PubMed]
Alfirevic A, Mills T, Carr D, Barratt BJ, Jawaid A, Sherwood J, Smith JC, Tugwood J, Hartkoorn R, Owen A, Park KB, Pirmohamed M. Tacrine-induced liver damage: an analysis of 19 candidate genes. Pharmacogenet Genomics. 17: 1091-1100, 2007.
[CrossRef]
[PubMed]
Carr DF, Alfirevic A, Tugwood JD, Barratt BJ, Sherwood J, Smith J, Pirmohamed M, Park BK. Molecular and genetic association of interleukin-6 in tacrine-induced hepatotoxicity. Pharmacogenet Genomics. 17: 961-972, 2007.
[CrossRef]
[PubMed]
Chatterjee PK, Yeboah MM, Dowling O, Xue XY, Powell SR, Al-Abeb Y, Metz CN. Nicotinic Acetylcholine Receptor Agonists Attenuate Septic Acute Kidney Injury in Mice by Suppressing Inflammation and Proteasome Activity. PLoS One. 7, 2012.
Chiavolini D, Alroy J, King CA, Jorth P, Weir S, Madico G, Murphy JR, Wetzler LM. Identification of immunologic and pathologic parameters of death versus survival in respiratory tularemia. Infect Immun. 76: 486-496, 2008.
[CrossRef]
[PubMed]
Davis KL, Thal LJ, Gamzu ER, Davis CS, Woolson RF, Gracon SI, Drachman DA, Schneider LS, Whitehouse PJ, Hoover TM, Morris JC, Kawas CH, Knopman DS, Earl NL, Kumar V, Doody RS. A double-blind, placebo-controlled multicenter study of tacrine for Alzheimers-disease. N Engl J Med. 327: 1253-1259, 1992.
[CrossRef]
[PubMed]
Fernandes-Alnemri T, Yu JW, Juliana C, Solorzano L, Kang S, Wu JH, Datta P, McCormick M, Huang L, McDermott E, Eisenlohr L, Landel CP, Alnemri ES. The AIM2 inflammasome is critical for innate immunity to Francisella tularensis. Nat Immunol. 11: 385-394, 2010.
[CrossRef]
[PubMed]
Field RH, Gossen A, Cunningham C. Prior pathology in the basal forebrain cholinergic system predisposes to inflammation-induced working memory deficits: reconciling inflammatory and cholinergic hypotheses of delirium. J Neurosci. 32: 6288-6294, 2012.
[CrossRef]
[PubMed]
Friedman A, Kaufer D, Shemer J, Hendler I, Soreq H, TurKaspa I. Pyridostigmine brain penetration under stress enhances neuronal excitability and induces early immediate transcriptional response. Nat Med. 2: 1382-1385, 1996.
[CrossRef]
[PubMed]
Gnatek Y, Zimmerman G, Goll Y, Najami N, Soreq H, Friedman A. Acetylcholinesterase loosens the brain’s cholinergic anti-inflammatory response and promotes epileptogenesis. Front Mol Neurosci. 5: 66, 2012.
[CrossRef]
[PubMed]
Jokanovic M. Medical treatment of acute poisoning with organophosphorus and carbamate pesticides. Toxicol Lett. 190: 107-115, 2009.
[CrossRef]
[PubMed]
Knapp MJ, Gracon SI, Davis CS, Solomon PR, Pendlebury WW, Knopman DS. Efficacy and safety of high-dose tacrine - a 30 week evaluation. Alzheimer Dis Assoc Dis. 8: S22-S31, 1994.
Krall WJ, Sramek JJ, Cutler NR. Cholinesterase inhibitors: A therapeutic strategy for Alzheimer disease. Ann Pharmacother. 33: 441-450, 1999.
[CrossRef]
[PubMed]
Mahawar M, Atianand MK, Dotson RJ, Mora V, Rabadi SM, Metzger DW, Huntley JF, Harton JA, Malik M, Bakshi CS. Identification of a Novel Francisella tularensis Factor Required for Intramacrophage Survival and Subversion of Innate Immune Response. J Biol Chem. 287: 25216-25229, 2012.
[CrossRef]
[PubMed]
Novosad J, Holicka M, Novosadova M, Krejsek J, Krcmova I. Rapid onset of ICAM-1 expression is a marker of effective macrophages activation during infection of Francisella tularensis LVS in vitro. Folia Microbiol (Praha). 56: 149-154, 2011.
[CrossRef]
[PubMed]
Pohanka M. Alzheimer’s disease and related neurodegenerative disorders: implication and counteracting of melatonin. J Appl Biomed. 9: 185-196, 2011a.
[CrossRef]
Pohanka M. Cholinesterases, a target of pharmacology and toxicology. Biomed Pap. 155: 219-229, 2011b.
[CrossRef]
Pohanka M. Acetylcholinesterase inhibitors: a patent review (2008 - present). Expert Opin Ther Pat. 22: 871-886, 2012a.
[CrossRef]
[PubMed]
Pohanka M. Alpha7 nicotinic acetylcholine receptor is a target in pharmacology and toxicology. Int J Mol Sci. 13: 2219-2238, 2012b.
[CrossRef]
[PubMed]
Pohanka M, Pavlis O. Neostigmine modulates tularemia progression in BALB/c mice. Afr J Pharm Pharmacol. 6: 1317-1322, 2012.
[CrossRef]
Pohanka M, Pavlis O, Ruttkay-Nedecky B, Sochor J, Sobotka J, Pikula J, Adam V, Kizek R. Tularemia progression accompanied with oxidative stress and antioxidant alteration in spleen and liver of BALB/c mice. J Microbiol. 50: 401-408, 2012.
[CrossRef]
[PubMed]
Shen H, Harris G, Chen W, Sjostedt A, Ryden P, Conlan W. Molecular immune resposnes to aerosol challenge with Francisella tularensis in mice inoculated with live vaccine candidates of varying efficacy. PLoS One. 5: e13349, 2010.
[CrossRef]
[PubMed]
Sun L, Zhang GF, Zhang X, Liu Q, Liu JG, Su DF, Liu C. Combined administration of anisodamine and neostigmine produces anti-shock effects: involvement of alpha 7 nicotinic acetylcholine receptors. Acta Pharmacol Sin. 33: 761-766, 2012.
[CrossRef]
[PubMed]
Teltingdiaz M, Lunte CE. Distribution of tacrine across the blood-brain-barrier in awake, freely moving rats using in vivo microdialysis sampling Pharm Res. 10: 44-48, 1993.
[CrossRef]
Tyagi E, Agrawal R, Nath C, Shukla R. Effect of anti-dementia drugs on LPS induced neuroinflammation in mice. Life Sci. 80: 1977-1983, 2007.
[CrossRef]
[PubMed]
Wang J, Chen F, Zheng P, Deng WJ, Yuan J, Peng B, Wang RC, Liu WJ, Zhao H, Wang YQ, Wu GC. Huperzine A ameliorates experimental autoimmune encephalomyelitis via the suppression of T cell-mediated neuronal inflammation in mice. Exp Neurol. 236: 79-87, 2012.
[CrossRef]
[PubMed]
Wilund KR, Rosenblat M, Chung HR, Vokova N, Kaplan M, Woods JA, Aviram M. Macrophages from alpha 7 nicotinic acetylcholine receptor knockout mice demonstrate increased cholesterol accumulation and decreased cellular paraoxonase expression: a possible link between the nervous system and atherosclerosis development. Biochem Biophys Res Commun. 390: 148-154, 2009.
[CrossRef]
[PubMed]
Zitnik RJ. Treatment of chronic inflammatory diseases with implantable medical devices. Cleve Clin J Med. 78: S30-S34, 2011.
[CrossRef]
[PubMed]
|
BACK
|